How to Fix Senior Living
A new task force's recommended urgent changes, and some reality checks
Given the steep number of COVID-19 deaths and cases in nursing homes and lack of PPE there; the recent inability to see loved ones in assisted living and retirement communities as well as the poor pandemic communication between many operators and families of their residents, is it any wonder that senior living (also called senior housing) now has a giant black eye?

Boomers in particular — children of most senior living residents and potential senior living inhabitants themselves — often have issues with the way the $250 billion industry is run and what it offers, or doesn’t.
For many, said Robert Kramer, the insightful founder and strategic adviser to the National Investment Center for Seniors Housing & Care (NIC), “they don’t want anything to do with it,” because of what’s happened during the pandemic.
Some boomers have seen senior living as senior dying.
In particular, boomers lacking personal experience with senior housing, Kramer said, “have mostly seen senior living as senior dying; that’s where you’re going to die.”
It’s why the International Council on Active Aging (ICAA) brought together 154 senior living industry leaders and analysts to form a task force and spent three months knocking out the new report: Creating a Path Toward the ‘Next Normal’ in Senior Living.
The ICAA report noted that the COVID-19 pandemic has “dramatically affected the operations of all senior living organizations, costing jobs, billions in lost revenue and the emerging effects of social isolation, declines in cognitive and physical function and loss of spiritual and social engagement.” It laid out what the task force said were six strategies to better serve residents, staff and families.
What 'The Next Normal' Senior Living Report Left Out
But the ‘Next Normal’ report left out one critical senior living topic: affordability.

I’ve pored through the ICAA study and its proposals, interviewed its key creators and other analysts and read all I could about what’s really happened at senior living facilities during the pandemic as well as what Americans think about this business.
I should really say businesses, because senior living is actually a spectrum of very different types of places to live when you’re older. They range from the high-end, for people who are generally healthy (active-adult communities and independent living) to continuing care/life plan communities (a mix of healthy people and less so) to places where people are typically the oldest and least healthy (assisted living, skilled nursing and nursing homes).
“It is absolutely a new day for the industry; a lot of us are struggling with what in the heck the future holds,” said Colin Milner, the ICAA’s CEO and founder and task force co-chairperson. “This is a potential reset moment.”
But it’s one for what Senior Living Foresight publisher Steve Moran calls “a pretty risk-averse industry.”
"The industry itself has allowed a widespread amount of confusion."
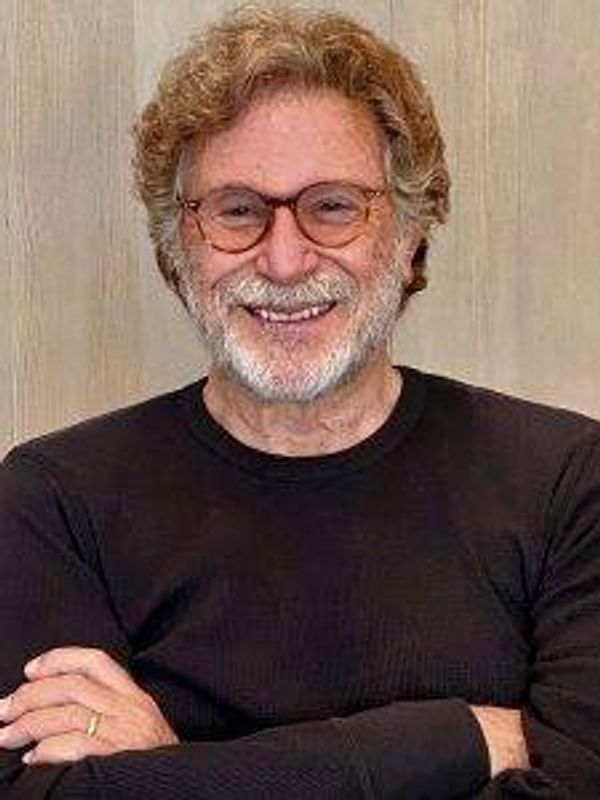
Ken Dychtwald, an ICAA report co-chairperson who is founder and CEO of the research and consulting firm AgeWave and co-author of “What Retirees Want: A Holistic View of Life’s Third Age,” said the task force especially focused on two things.
One was: “How do we optimize the health and wellness of residents and staff? And that’s more than just COVID safety… We really need to step up health and wellness about five levels,” said Dychtwald.
The other: “The industry itself has allowed a widespread amount of confusion” about its varied types of facilities and communities, Dychtwald said.
Here are the six key ways the ICAA report said senior living needs to change, how they may or may not happen and, to borrow from Sherlock Holmes, “the dog that didn’t bark” (the unspoken affordability issue).
1. Design, Re-design and/or Renovate Exteriors and Interiors of Buildings
This is about ways to minimize COVID-19 exposure, enhancing safety and providing outdoor space for programs, social connections and individual pursuits.
Among the task force’s recommendations: Install air filtration systems to reduce airborne viral transmission; minimize touch where possible (such as automatic doors and voice-activated lighting); create “isolation-friendly” areas; add Juliet balconies to allow for outdoor connection with others and reimagine outdoor spaces to reduce social isolation and provide places for individuals, groups and visitors.
Some of these things have already started happening to help avoid contagion risk. For instance, Willow Valley Communities, in Lancaster, Pa., has built climate-controlled “Connections Cottages” to let visitors separated by a window pane speak to residents.
“If I’m a person moving into a community, one of the questions I would have is: How is your building ‘well’ and what will that mean for me as I move in here?” said Milner.
Dychtwald noted that redesigns and renovations would mean a new way for people to live in senior living.
Our Commitment to Covering the Coronavirus
We are committed to reliable reporting on the risks of the coronavirus and steps you can take to benefit you, your loved ones and others in your community. Read Next Avenue's Coronavirus Coverage.
“There’s always been an expectation that one of the attractions was community rooms where they dined together or watched TV or attended yoga classes,” he said. “That’s all got to be rethought. It may be that more has to occur in rooms, or in a custom-service fashion.”
One possibility: smaller footprints. That could mean making or converting assisted living facilities into a “neighborhood model” with four to 20 beds in each building.
Moran told me that entrepreneur Gene Guarino hopes to build 1,000 “residential assisted living academies” by the end of 2021.
Another possibility: bringing the community aspect of senior living to older adults in their own homes.
That’s what Kendal, an owner of locally owned not-for-profit retirement communities, does with its Kendal at Home affiliate. It provides home care, access to transportation, nutrition counseling and other services.
“I believe our sector has the aptitude and responsibility to take the whole and break it into smaller components to be available to individuals’ homes,” said Sean Kelly, Kendal’s president and CEO. “You don’t necessarily have to have everyone living in the same place, with big entrance fees.”
"They never knew they had so many residents who could sing and dance and lecture and teach and cook."
Reality check: The average nursing home in big metro areas is 40 years old, said Kramer. These homes were “designed with narrow hallways and as many as three to four beds to a room,” he noted.
So, “it’s going to be really tough” to renovate places like that, said Moran.
2. Develop Purpose-driven, Caring, Passionate Staff
This recommendation included evaluating the feasibility of “universal worker” staffing; replacing some part-timers with full-time people and providing equitable wages and benefits.
Universal staffing, Kramer said, means consistent, efficient staffing where employees “are able to do more than one thing; they can cook, clean and care, as well as be there as a friend.”
Treating staff better, said Moran, is also about catering to their needs, especially during stressful times like the pandemic. That might include setting up day care for their children. Or giving them meals to take home to families. Or creating on-premises stores where staffers (and residents) can save on groceries.
As I wrote on Next Avenue, some savvy independent living operators have been finding clever ways to grow social engagement with residents and staff during the pandemic.
Moran told me: “One thing I’ve heard, and I love, is that they never knew they had so many residents who could sing and dance and lecture and teach and cook. What it tells me is there is all this untapped talent in communities among staff and residents.”
Reality check: Will senior living operators, many of whom are already feeling pinched, spend the money on higher wages and better benefits for staff? If they pass on the extra costs to residents, will those people have the money to pay for them?
3. Provide Technology to Increase Connections, Aid Efficiency and Optimize Health
The task force had 33 recommendations here, since senior living operators have done a pretty lousy job, overall, giving residents tech access and training so they could communicate with families and medical professionals during the pandemic and receive telehealth.
According to Kramer, “health care has always lagged behind other sectors in technology and senior housing has lagged behind health care.”
Among the task force’s suggestions: explore technology solutions to meet the needs of residents, family members and staff; provide high-speed internet; build telehealth into daily operations; provide tablets and computers to all residents; survey residents and staff about their tech knowledge and abilities; train some residents to be tech mentors; hire a tech support staffer; show residents how to use smartphones to track their health and expand telehealth practices to include mental health and rehabilitation practitioners.
Dychtwald said providing the ability, and training, for residents to conduct telehealth appointments has become essential.
“When older people are in need of medical care and they don’t know how to how to use telemedicine and their rooms aren’t wired and there’s no staff education program for digital tech, that can be fatal,” he said.
Reality check: Senior living analysts doubt that all operators will be able to afford supplying residents with tablets, computers or smartphones.
“I think it’s dependent on size,” said Milner. “If I have a community like The Villages, with a hundred thousand people, it’s probably not going to happen. But if I have one hundred or two hundred residents, the likelihood of that happening is much more.”
Some residents or families might be charged to help pay for receiving the technology, he added.
4. Develop the Culture of Positive Aging, Framed by all the Dimensions of Wellness
This section spoke to a core ICAA belief: wellness.
The task force recommended, among other things: elevating the wellness/lifestyles leader to the management team; developing a model of “whole-person wellness, purpose and meaning;” developing knowledge of individual residents’ interests, wellness goals, strengths and skills; considering offering rent discounts for those participating in wellness programs and re-examining ageist assumptions that underestimate the physical and cognitive abilities of older adults, preventing them from performing at their true potential.
Too often, senior living operators and staffers 'come out with a sense of you’re in decline and we want to pinpoint your decline.'
Lisa Marsh Ryerson, president of the AARP Foundation, thinks senior living activities directors need to become “purpose matchmakers” for their residents.

But wellness includes mental health as well as physical health.
The isolation many senior living residents have been feeling has been extremely rough on them.
A study of one suburban Chicago nursing home found that 23% of residents lost over 5% of weight, partly because group meals were replaced with in-room delivery.
Reality check: Too often, Kramer said, senior living operators and staffers “come out with a sense of you’re in decline and we want to pinpoint your decline.”
But, he added, “I think people want to be known by their gifts, talents, passions and desires to grow and learn. That means asking them when they move in and when they live in the community: ‘What gifts will you bring?’ What’s next for you? How do you want to grow and learn?’”
5. Establish Trust by Being Prepared to Respond to Emergencies and Unexpected Events
This is partly about transparency, something sorely lacking at many senior living facilities and communities during COVID-19 — especially nursing homes and assisted living. And it’s partly about preparedness, which has also been in short supply.
Among the task force’s recommendations: relay information to families and referral sources through each property’s website, Facebook and social media messages and email; establish a staffed phone hotline to answer calls during a disaster or emergency; build pipelines to make sure there is an adequate supply of personal protective equipment (PPE) on site; upgrade staff training to insure competence in infection control.

These ideas are especially important for skilled nursing and assisted facilities. They’ve had great difficulty getting enough PPE and have also had the worst coronavirus results during COVID-19.
In NIC reports, roughly 4% of residents of nursing homes, 3.3% of those in memory care and 2.4% of those in assisted living have tested positive, while only about 0.3% of those in independent living have. More than 95% of people with Alzheimer’s and other forms of dementia have another chronic health condition, raising their likelihood of complications from COVID-19, according to the Alzheimer’s Association.
By contrast, said Milner, “there are many senior living communities that had zero cases” of the coronavirus.
Reality check: PPE and COVID-19 testing depend greatly on government support for the senior living communities. But in the pandemic, said Milner, most of the PPE has gone to hospitals. And, according a Time investigation, the government’s PPE supplies for long-term care facilities have been limited in quantity and sometimes unusable.
LeadingAge, a trade group for nonprofit senior care providers, recently said that three of its members are closing due to coronavirus-related costs.
6. Update Perceptions to Reinforce the New Value Proposition of Each Type of Senior Living
Are the problems facing senior living operators really about perception? Or reality? Or a little of both?
The task force recommended, among other things, commissioning a study comparing social isolation in senior living compared to those living elsewhere; contrasting life experience, infection and death rates among similar-aged groups in independent living, assisted living and memory care against others; possibly retiring the term “retirement community” and the words “senior” and “assisted living” and working to alter the public’s perceptions of aging.
"Now, with COVID-19, I think the industry as a whole has a serious PR issue that has to be addressed.”
Reality check: Even the strongest advocates for senior living worry about how to change perceptions — especially among boomers.
“I think the perception of senior living is based on a very dated model,” said Milner.
And, he added, changing perceptions will be the hardest thing to change for the senior living industry. “Perceptions of senior living weren’t that great to start with. And now, with COVID-19, I think the industry as a whole has a serious PR issue that has to be addressed," Milner said.
Dychtwald agreed.
“I think [senior living operators] are wildly unprepared for the next generation,” said Dychtwald. He’s talking about boomers in their late 50s and 60s.
“I have dealt with many of the companies and investors involved in this sector and have not been impressed how deeply they understand how different boomers are with the people they’re now serving,” Dychtwald said.
The owners of these communities and facilities, Dychtwald said, “have got to remove the negatives or they’ll be out of business.”
One More Needed Change: Affordability
Finally, there’s the issue of affordability.
The 2019 State of Senior Living survey of 200 industry professionals by the Perkins Eastman planning and design firm found that 90% of respondents anticipated financial strains on their consumers as their primary concern.
Three years in a private room in a nursing home costs more than a total of $300,000, according to the Genworth Cost of Care Survey. That’s way more than what most people in their 50s and 60s have in retirement savings, notes the National Institute on Retirement Security.
These days, if you have enough money, you can afford to live in an active-adult community or an independent living development. Jimmy Buffett’s Margaritaville-themed communities (which cost around $250,000 to $400,00 plus monthly maintenance fees) have been wildly popular. But not everyone has the scratch.
And if you’re very poor, you can generally get Medicaid to cover the cost of living in a nursing home.
But what about the people Kramer calls “the forgotten middle?” Those who are without much in retirement savings, but have too much income and assets for Medicaid.
The ICAA task force didn’t offer any recommendations. “To be frank, that was an oversight,” said Milner, who concedes that helping the middle class “needs to change.”
It’s possible that building redesigns, smaller developments, better technology and telehealth will help bring some costs down for residents.
But Kramer thinks this is an industry that’s due for disruption, which may lead to more affordable options.
“There’s going to be a shakeout in senior housing and the care space and in skilled nursing,” he said. “Our sector is ripe for outside disruption.”
And who might be those disruptors?
Kramer looks to businesses ranging from health insurers to the likes of CVS and Walmart, who understand and cater to older customers. Some of these companies might become partners; some could turn into senior living developers.
“They’re all nibbling at the edge,” Kramer said.
Abby Miller Levy, co-founder of the new Primetime Partners longevity and older adults investment venture capital fund (a former wellness executive), agrees.
“I’m seeing a lot of idea thinking in how we design more modular accommodations where we can push down the price and how to use technology to make it more affordable," she said.
By 2029, according to NIC, 54% of people 75 and older will be financially ill-prepared to pay for senior housing.
“I believe we have to think of serving the middle as a new paradigm altogether,” said Kelly.


