Home Technology for Older Adults: Safety or Intrusion?
As caregivers monitor patients, privacy becomes an issue
(This article previously appeared on the site Providermagazine.com.)
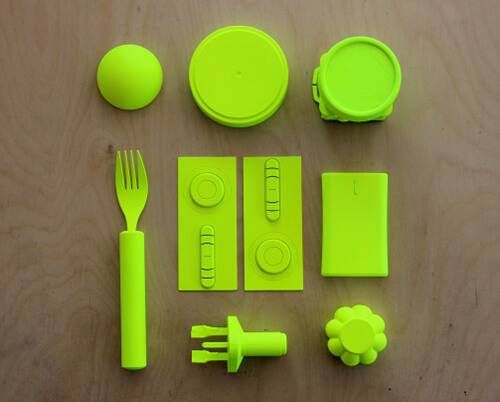
His family meant well. Thomas, aged 70, lives on his own since the death of his wife last year. His children send him smart devices to track and monitor his diet, health and sleep from a distance — respectively, a fork, a cane and a bedpost.
But Thomas craves his independence. He struggles with the order and rules imposed on him by the objects that are meant to make his life easier. Eventually he outwits these “smart objects” by leaving the fork in a plate of salad while he eats his bangers and mash (he's British), by bribing his younger neighbor with a beer to take the cane out for a walk and by placing enough books — one of them cleverly titled Why Should Anyone Be Led by You? — on the bed to fool the device into thinking he’s asleep.
The above scene, from a video by Superflux Lab called “Uninvited Guests," says it all. It provokes questions about how people want to live and grow old in an increasingly technologically mediated world. Yet these devices are coming, so long-term and post-acute care providers should start preparing. Time will tell if these devices are a help or a hindrance.
There’s even a term for these health care devices that are wirelessly connected to the cloud: The Internet of Caring Things.
Wireless Connections With a Purpose
Imagine a home where hidden sensors in the walls can predict a fall weeks before the event occurs, the front door can be unlocked by someone who is immobilized upstairs and a cup can call the ambulance if an elderly person with congestive heart failure or chronic kidney disease is in severe danger of becoming dehydrated or malnourished.
Welcome to the Internet of Caring Things — a buzzword for those in the technology industry. Examples that have already hit the mainstream include the Fitbit wearable fitness tracker and the Nest smart thermostat. There’s even a seminar on the topic at South by Southwest, a “Woodstock” for early adopters who openly welcome interactive technologies.
Separately, these innovations may seem frivolous, but collectively they represent a revolution in how health care is managed: turning a check-up into a 365/24/7 process, not an annual event.
“The Internet of Caring Things is about purposeful connections,” says Dr. Hanson Lenyoun, a former surgeon and alum of Harvard University and Columbia University College of Physicians and Surgeons. Lenyoun is now head of health at consumer health startup Mark One, the makers of Pryme Vessyl, an intelligent cup that automatically tracks and displays an individual’s hydration needs.
“Often we speak about it as a gimmick — smart this and dumb that — why do you need to turn your coffeepot on from your bed? But it’s about much more than that. In my world, it’s about tracking vital signs and collecting data to facilitate change and improve people’s health or prevent disaster,” Lenyoun says.
‘Tea. Earl Grey. Hot.’
Cisco, a worldwide information technology (IT) company headquartered in San Jose, Calif., estimated in a white paper that 100 “things” are coming online every second. Gartner, an IT research and advisory company in Stamford, Conn., wrote in one study that in 2005, there were 2.5 billion connected devices — most of which were personal computers, smartphones and tablets — but by 2020, there will be 20.8 billion — most of which will not be the aforementioned and familiar technological trifecta.
“These results are building on the fact that technology, according to Moore’s Law, has doubled every two years as the cost has come down,” says Senior Vice President of Thought Leadership at AARP Jody Holtzman.
“The Internet of Caring Things is just a label for the fact that everything about your home, from lights to water to heat to computer to cell phone, is going to be connected so data and communication can flow amongst and in between the varied devices,” Holtzman notes.
If it sounds Orwellian, think again. An AARP and Georgia Tech study called Project Catalyst found that when 92 older consumers were given one of seven popular fitness tracking devices to use in their daily lives for six weeks, 42 percent of participants said they planned to continue to use such a device in the future.
“My touchstone is Star Trek,” says Holtzman. “An exciting future is ahead where one can speak into air, ‘Computer: Tea. Earl Grey. Hot.’ Or, ‘Tell me when we get to universe 06370.’”
Not Typical Retirement Living
For residents living in TigerPlace, the future is now, although from general appearances TigerPlace appears to be a typical nursing care center.
Named after the University of Missouri (MU) mascot, the tiger, it’s a specially designed elder housing project started in 2004 by the MU Sinclair School of Nursing and designed by MU faculty working with the Americare Corp. of Sikeston, Mo.
Inside the building are 32 private apartments with fully accessible bathrooms, kitchens and screened porches. Private garages and a private dining room for special family occasions are available, as are common spaces such as a living room, dining room, library, sports bar, gym and beauty shop. There’s even a veterinary medicine clinic. And people can live there through the end of life, too.
Yet purposely disguised within and throughout the well-painted and decorated interior is a wireless sensor system to help detect illness and keep the residents out of the hospital.
Sensors include one placed under a patient’s mattress to detect restlessness, as well as abnormal breathing and pulse rates when sleeping, and another to monitor a patient’s gait to help predict falls. A smart carpet is under development for recognizing falls. The current system, which is in additional pilot studies in 12 assisted living facilities in Missouri, averages about $200 a person per month. Eventually the system will also be offered to private homes for a similar fee.
Marilyn Rantz, TigerPlace’s executive director, says that bed sensors can predict illness 10 days to a month out. Similarly, falls can be prognosticated two weeks to one month ahead of the actual event. Their studies have shown that the increased length of stay in TigerPlace doubled for people who had the sensors installed in their apartment, compared with those who opted out.
Person as Client, Not Just Patient
Sometimes all it takes is looking at something and someone in a different way.
“Frankly, most Internet things are being designed for demographics other than older adults, such as the Millennial market,” says Scott Moody, previous co-founder and CEO of AuthenTec, the fingerprint recognition device known as TouchID that is seen on all Apple smartphones and tablets. “Part of our approach is to repurpose these devices designed for others to make the lives of older adults better, simpler and healthier.”
Enter Moody’s new company, K4Connect, which caters to both senior living community residents (K4Community) and, soon, to the professional home care community (K4HomeCare) and those living independently at home (K4Life). Essentially, via a smart tablet, an individual’s apartment is turned into a smart home. The thermostat automatically lowers at night and rises in the morning to promote better sleep. The bathroom and bedroom lights turn on when someone gets out of bed, so people can safely traverse from bed to bathroom.
A Fitness tracker is integrated with apartment activity so residents can track their progress and goals. Dining menus and activity calendars are easily accessed. The tablet can also be used as a phone to call loved ones and as a television remote.
“One of the challenges we see of those pursuing this market is that they pursue it similar to the way they did other markets, developing thousands of unique standalone products and applications,” Moody says. “But who is going to manage all that, bring it all together?
“These products go well beyond what is sometimes no more than a novelty to some, but they provide real utility to our clients. For example, if someone rings a doorbell, it shows up on the tablet, and one can unlock it from the bedroom meters away,” says Moody. “For you and me, that’s nice. We don’t have to get off the couch to let in a friend. But if you live with a disability, are more prone to falling or if you’re in a wheelchair, this is an incredibly important product. It provides more utility and true value to older adults than [to] a 25-year-old.”
And not just the client benefits from the service, he says.
“We look at a person living with a disability not as a patient but as our client. We provide a great experience just like you would expect of any other consumer offering,” says Moody. “If we do well by our clients, the benefit flows to others in their ecosystem such as their family and community staff.”
The website claims that K4 benefits operators by “improved customer/family satisfaction, reduced staff turnover, increased revenue and cost savings.”
Cup Half-Empty or Half-Full?
“The potential advantages of these devices are clear and many,” says Lenyoun. “They can make it easier for users to monitor their own health or the health of loved ones from afar, help improve health and well-being in general, decrease stress, increase care, decrease cost, improve outcomes and make life easier for anyone, regardless of their age.”
Lenyoun’s device is one of those why-didn’t-someone-think-of-this-before inventions: a connected cup called Vessyl that automatically calculates how much liquid a person has drunk and how much more is needed to maintain optimum hydration levels.
It’s much more than simply getting eight glasses of water a day, explains Lenyoun.
“This is very relevant for the elderly as the thirst drive wanes with age, so that population is at real risk of ending up dehydrated,” he says. “Dehydration is dangerous for them, and it has a big impact on our medical system — there are more than 500,000 hospitalizations each year specifically due to dehydration.”
While it wasn’t specifically designed for that purpose, Pryme Vessyl could certainly be used in a skilled nursing center or assisted living environment.
Fluid consumption tracking is important in many disease states, such as congestive heart failure and chronic kidney disease. The case can also be made for the device to track liquid (or thickened liquid) intake for patients with dysphagia [difficulty swallowing].
“I remember back to my time on the hospital wards, watching nurses spend exorbitant amounts of time measuring out and writing down fluid intake for patients and thinking there must be a better way. Now there is,” says Lenyoun.
One Size Does Not Fit All
Yet these computerized devices do pose some challenges.
For one, elders are not a homogeneous group — individuals live in various health and living conditions. As such, the Internet of Things must fit into their lives, not the other way around.
“We must consider the aging trend from a wider perspective than a simple end-user versus a new technology,” says Nicola Palmarini, technology advocate for IBM Research. “It involves a value chain of stakeholders, from relatives to care providers and caregivers to the insurance industry, all connected to the Internet of Caring Things.”
Acceptance by this population is a key issue. Some may see these devices as an intrusion on their privacy. Others may see any outward signs of using this technology as a public symbol of their age and frailty and so avoid their use for that reason.
The unknown may also be a bit scary — elders may be concerned about not being able to properly use the technology or trigger false alarms. Finally, cost can be a consideration; they may view these devices as too much of a luxury to spend money on.
“The challenge becomes helping the elderly easily adapt to a technology-driven world, prolong their independence, stay more connected with friends and family and help manage life’s everyday decisions,” says IBM Accessibility Senior Technologist Susann Keohane.
Mind the Data Dump
Clara Berridge, a post-doctoral fellow at Brown University’s Center for Gerontology and Health Care Research, offers further perspective.
“As a gerontologist, I’m interested in how technology will affect older adults and their caregivers, which is actually quite different from the aging market. Companies know that family members and provider organizations are their market, so there’s little incentive to design for older adults. And older adults are harder to design for precisely because they are a diverse population with needs that are more multifaceted than those who are making purchasing decisions,” says Berridge. “My research indicates that older adults are interested in safety, control, human contact and relationships, privacy and autonomy. Caregivers and organizations are more likely to prioritize risk management and efficiency.”
Berridge also cautions against “data dumping,” or avoiding the deluge of data that comes from the constant monitoring of individuals. Not every piece of information gleaned will be of practical use for the physician or caregiver.
“Currently, much of the data on movements, sleep, biometrics, potential falls and what have you come to the end user in the form of an avalanche,” says Berridge. “In nursing homes, certified nurse assistants often report alert burnout — they reasonably stop responding after so many nonsignificant alerts have needlessly disrupted their work.”
Man Versus Machine
As the character Thomas illustrated in the video described at the beginning of this article, an inevitable tension occurs between values of privacy, autonomy, independence and safety when new forms of monitoring are introduced into a care relationship.
“We need to get in touch with what privacy means to elders and why it matters, quickly,” says Berridge. “To make this concrete, what if a family member seeks an explanation for an activity picked up by the connected device that the older adult wants to keep private for their own reasons? One of my 80-something-year-old research participants who discontinued a sensor-based activity monitoring system because she felt ‘spooked out’ and ‘followed,’ asked what happens when she’s in the company of a romantic partner and doesn’t want to be questioned by her children when they notice a change in activity in her home?”
Berridge notes in her studies that having one’s movements monitored can lead older adults to develop a sense of hypervigilance and behavior change, which actually threatens their autonomy. She also foresees significant ethical problems with a medical adherence solution that remains to be mainstreamed.
One proposed solution to medication management has been the idea of ingestible sensors, or “smart pills,” which again raises serious privacy and personal autonomy problems, such as informed consent (for example, “You can stay home and use this device or go to a nursing home”).
“Power dynamics are always at play in passive monitoring, and we need to keep a close eye on whose priorities are [being] designed for and addressed in our solutions, as well as make sure breathing room remains,” Berridge cautions.
Proactive Rather Than Reactive Health Care
Challenges also remain for the technology and health care industry. Currently, there’s little oversight of the Internet of Caring Things. In February 2015, the Senate Committee on Commerce, Science, and Transportation convened its first meeting on the topic. Lawmakers walk a fine line between being sensitive about regulations stifling innovation while trying to understand the implications of developing technologies. That includes ensuring that the technology infrastructure is adequate to support and keep secure the traffic volume of these devices.
“There are a lot of regulations that the government has done a good job at developing: FDA [Food and Drug Administration] certification, PCI [payment card industry] compliance, HIPAA [the Health Insurance Portability and Accountability Act]. But it shouldn’t overdo it — it’ll slow things down,” says David Inns, CEO of GreatCall, a company that focuses on active aging technology (customized wearables, smartphones, flip phones, apps and home devices) for older consumers to keep them independent longer.
“The Internet of Caring Things makes it possible — on an unprecedented level — to collect, transmit and store massive amounts of data about people. The large-scale collection of medical and health data by powerful companies has been less than transparent to the average customer,” he says.
An incentive system needs to be placed in health care to promote data sharing, experts say.
"If health care companies want providers to collect more data about their patients, they will eventually incentivize it in a way that patients will feel,” says Berridge. “Eventually, this will have the effect of pressuring patients, possibly financially, to consent to have information about themselves shared with their providers that they would prefer not be shared. Why not have your Fitbit data automatically uploaded to your electronic health record?”
Health care will also need to do a paradigm shift so care provision will be more about prevention rather than treatment and cure.
“The current state of aging and senior care is reactive — providers race from one person to another fighting fires,” says Stephen Johnston, co-founder of Aging 2.0, a global network of innovators in aging. “We’re seeing a shift to make care more proactive, so providers can do data-driven triage, predict situations such as falls ahead of time and provide better care at lower cost.”
Here to Stay
Although the term “The Internet of Caring Things” has not yet made it into the lexicon, these devices are already here, and they’re here to stay.
“In the next five years, it’ll become the norm in terms of expectations (location, tracking, planning, scheduling and available profiles),” says Johnston.
Long-term and post-acute care providers need to start having conversations about these devices, and it will impact their caregiving.
“The insertion of the word ‘care’ into the Internet of Things is meaningful. We generally understand that care involves physical, socio-emotional and monitoring practices,” says Berridge. “Which elements of care are addressed through the Internet of Things? Well, monitoring. So either the Internet of Caring Things is a misnomer or we are redefining the meaning of care. But if we’re imagining that care is equivalent to monitoring, older adults are going to get the short end of the stick.”
Or refuse to use the electronic stick altogether, like Thomas. (See the video about him here.)

