Does COVID-19 Vaccine Shopping Make Sense?
People increasingly have a choice, so here's what experts say about selecting your jab
Anywhere you go these days (if you go anywhere), you can't help but overhear people swapping vaccine stories. Initially it was, "Did you get your shot?" But as three different vaccines became available in the U.S., the talk has shifted to which vaccine — and a lot of armchair analysis of which is "the one" to get.
The conversation took another turn in April, when news spread that six women — between 18 and 48 years of age — who had received the Johnson & Johnson COVID-19 vaccine had developed serious blood clots, one of them fatal. The J&J "jab" had been the new darling of the rolled-up sleeve set because it was the only approved vaccine that required just one shot.
For context, fewer than one in a million vaccine recipients were beset by the clotting disorder, but even before the Centers for Disease Control and Prevention (CDC) recommended a "pause" in use of the J&J vaccination for further study, some who had been holding out for the single dose shot began jumping ship.
You're more likely to develop blot clots from contracting the virus itself than from taking any currently approved vaccine.
At the Walgreens pharmacy in Greenville, N.Y., where pharmacists were administering the more available Pfizer vaccine, appointments for COVID-19 shots for a single day in April jumped from 34 to 116 after the Johnson & Johnson blood clot news broke.
Following a review of the data, the CDC recommended resumption of its use, stating that "the J&J/Janssen COVID-19 vaccine's known and potential benefits outweigh its known and potential risks."
To underscore that finding, a study published in mid-April from Oxford University suggests that you're more likely to develop blot clots from contracting the virus itself than from taking any currently approved vaccine.
You Can't Predict Which Vaccine You'll Tolerate Best
Reactions to any vaccine are highly individualized, and COVID-19 shots are no different. What leads to a mild headache in one person can cause days of body aches and fevers for another.
Kimberly Ayers was lucky. At 62, the retired journalist wrangled a spot in Pfizer's Phase 2/3 clinical trial in Long Beach, Calif. Some of the 29,000-plus participants got placebos in the double-blind study, but Ayers got the real vaccine, which soon became apparent.
She says she had some minor arm soreness after the first shot, but the second shot brought on general fatigue and a 99-degree fever that lasted about half a day.
"I'm absolutely good with it," says Ayers, who is relieved to be "vaxed." While she still wears masks and follows social-distancing guidelines, she's feeling confident enough to make travel plans again.
Eight hundred miles to the east, her longtime friend, Faye DeHoff, had a different experience. She also got the Pfizer vaccine, but the second shot packed a wallop.
"It was like I'd been hit by a truck and then run over three times," the 68-year-old retiree recalls. DeHoff suffered debilitating body aches and dizziness. It was three days before she felt like getting out of bed.
"People should not fool around. This is a very deadly virus and people should get vaccinated as soon as they can."
But there's a big difference between the two women: DeHoff suffers from Lupus, an auto-immune disorder that can exacerbate reactions to vaccinations of all sorts.
DeHoff says she discussed with her doctor the advisability of getting the COVID-19 shots and decided to give it a go. She now admits she'll have second thoughts if she needs another vaccine dose down the road.
Health experts say cases like DeHoff's demonstrate why it's so important that healthy people get vaccinated to protect those who can't.
Experts are increasingly skeptical that "herd immunity," the holy grail that physicians have been hoping would put the brakes on the spread of the virus, can be attained in the U.S. That makes it potentially even more important that people not hold out for a specific vaccine when another brand is available sooner.
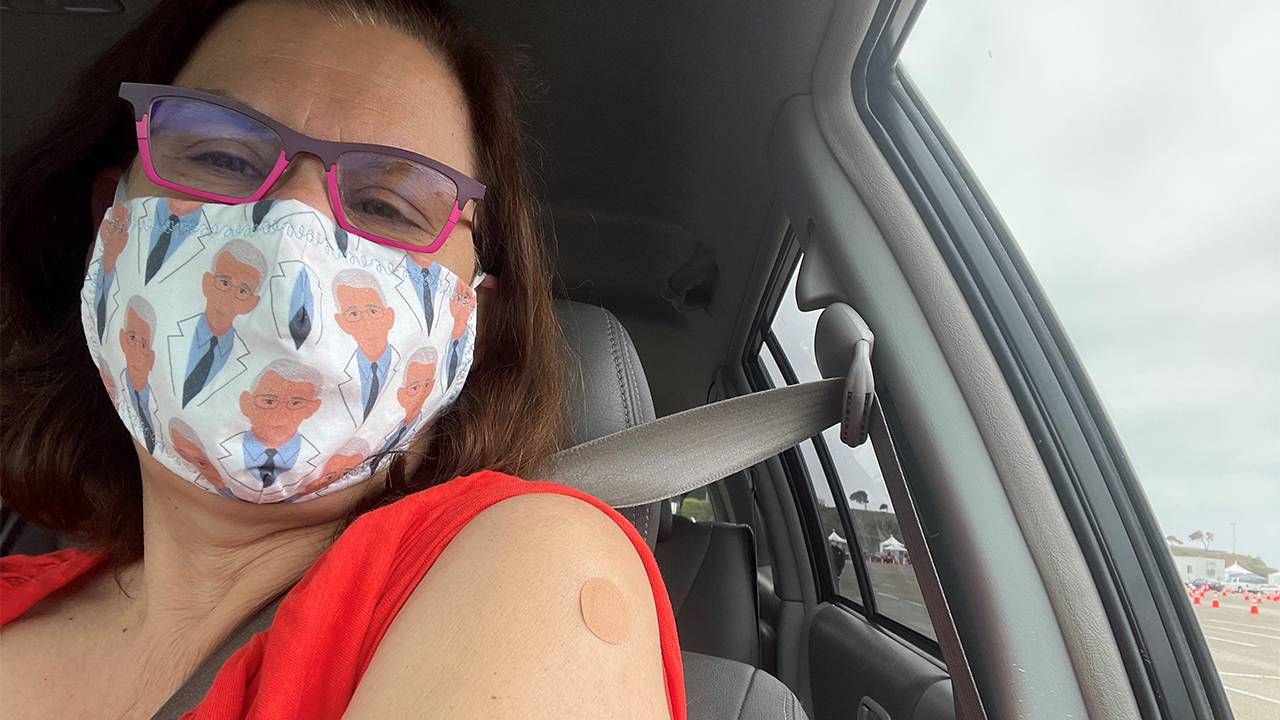
Lisa Aliferis, of Oakland, Calif., made it her personal mission to get her first vaccine dose on April 1, the first day the state lowered its eligibility bar to below age 65. She took to Facebook immediately, showing off her vaccination "badge," hoping to encourage others to get inoculated. Aliferis says she was a vaccination "hunter," not a shopper.
"People should not fool around," says Aliferis, 60, who is a senior communications officer at the California Health Care Foundation, a non-profit that aims to improve the quality of health care, especially for low-income residents. "This is a very deadly virus and people should get vaccinated as soon as they can," she says.
5 Frequently Asked Vaccine Questions
1. How many types of COVID-19 vaccines are available in the U.S.?
Three vaccines have been approved for use in the U.S.
The Pfizer-BioNTech is the most commonly administered shot so far, with the Moderna vaccine a close second and the Johnson & Johnson single-shot vaccine, also known as the Janssen vaccine, a distant third— partly because it was the latest to be approved. Nearly 200 vaccines are being tested in laboratories for future use and 13 are currently in circulation worldwide.
2. What are the similarities and differences between the vaccines?
The vaccines all work by harnessing your body's natural defenses to fight the invading virus. Both the Pfizer and Moderna vaccines were developed using newer techniques to produce a vaccine type known as mRNA. These contain genetic "instructions" for our native cells to produce proteins and lymphocytes that will fight future incursions by the virus.
The J&J shot is a more conventional "vector" vaccine. It contains a small amount of inactive material from the COVID-19 virus itself that prompts the body to build defenses similar to those produced by mRNA vaccines.
Clinical trials have shown slight differences in performance. Pfizer and Moderna both claim their vaccines are more than 90% effective at preventing a COVID-19 infection with symptoms. The J&J vaccine is reportedly 66% effective at preventing disease, but 85% effective at preventing illness serious enough to require hospitalization.
Our Commitment to Covering the Coronavirus
We are committed to reliable reporting on the risks of the coronavirus and steps you can take to benefit you, your loved ones and others in your community.
Read Next Avenue's Coronavirus Coverage
That could be an important distinction for you, depending on your current state of health and personal objectives. Is it important that you not get sick at all, or could you weather a mild case, just as long as you stay out of the hospital?
3. How long do the vaccines protect you?
The jury is still out. Recent studies suggest that the Pfizer and Moderna vaccines should offer about six months of protection. That estimate could be "on the conservative end," Dr. Stella Safo, assistant professor of medicine at Mt Sinai Hospital Medical Center in New York City, told the BBC.
Safo said she expected the picture to become clearer by this fall, but that it's unrealistic to think your first round of vaccinations will be all you need. "We don't know in a couple of months what the scenario will be," she said, "and so you should expect that you may need a booster."
4. Are the current vaccines effective against new virus variants?
This is another aspect that's still unclear. Early indications are that the vaccines offer at least some protection against current variants, but it's important to note that the virus will continue to mutate and the more people who have it, the more variants are likely to be produced (another reason to get as many people as possible vaccinated).
Clinical trials of the Pfizer and Moderna vaccines were conducted largely before the new variants appeared. All the major vaccine manufacturers say they're working to update their products to accommodate new variants.
5. Can I still get COVID-19 after being vaccinated?
It's possible, but unlikely. None of the vaccines are 100% effective in all cases. In mid-April, the CDC reported that 5,800 U.S. residents had contracted the virus after being fully vaccinated. Seventy-four of those "breakthrough" cases were fatal.
These are very small numbers compared to the more than 200 million doses delivered. That's about 27 people out of every million vaccinated or less than your chances of dying in a car accident as a passenger in the next year.
The bottom line message from public health experts continues to be: any COVID-19 vaccine is better than no vaccine. Or as Aliferis puts it, "The best vaccine is the one you can get."

Read More

