The Coming Wave of Nursing Home Closings
What COVID-19's effects mean for current and prospective residents and their families
More than 61,000 nursing home residents have died from the coronavirus since the pandemic began, 40% of all COVID-19 deaths. What's likely to come next: a wave of nursing home closings.

In an August 2020 survey of nursing home operators by the American Health Care Association (AHCA) and the National Center for Assisted Living (NCAL), 72% of respondents reported an inability to maintain operations through 2021; 40% said they won't last another six months.
"For many Medicaid patients, nursing homes are the only place they have to go."
Said Joe Steier, president/CEO of Signature HealthCARE, which operates 112 long-term care facilities in 10 Southern states: "The COVID pandemic was a black swan event no one was ready for that has resulted in the largest loss of beds in the country's history."
Congress and the Trump administration have given the nation's 1.2 million nursing homes roughly $7.5 billion in relief and Paycheck Protection Program money.
While older adults and nursing homes are at risk from the coronavirus pandemic, long-term care services and supports (LTSS) industry groups are signaling dire warnings about the continuum of care for the nation's rising older population.
"More than half of adults aged sixty-five plus require some form of LTSS as they continue to age. And the likelihood of need for care, and level of care needed, increases with age," said Lisa Sanders, a spokesperson for Leading Age, a 5,000-member advocacy organization serving nonprofit long-term providers and affordable housing for low-income older adults, in an email interview.
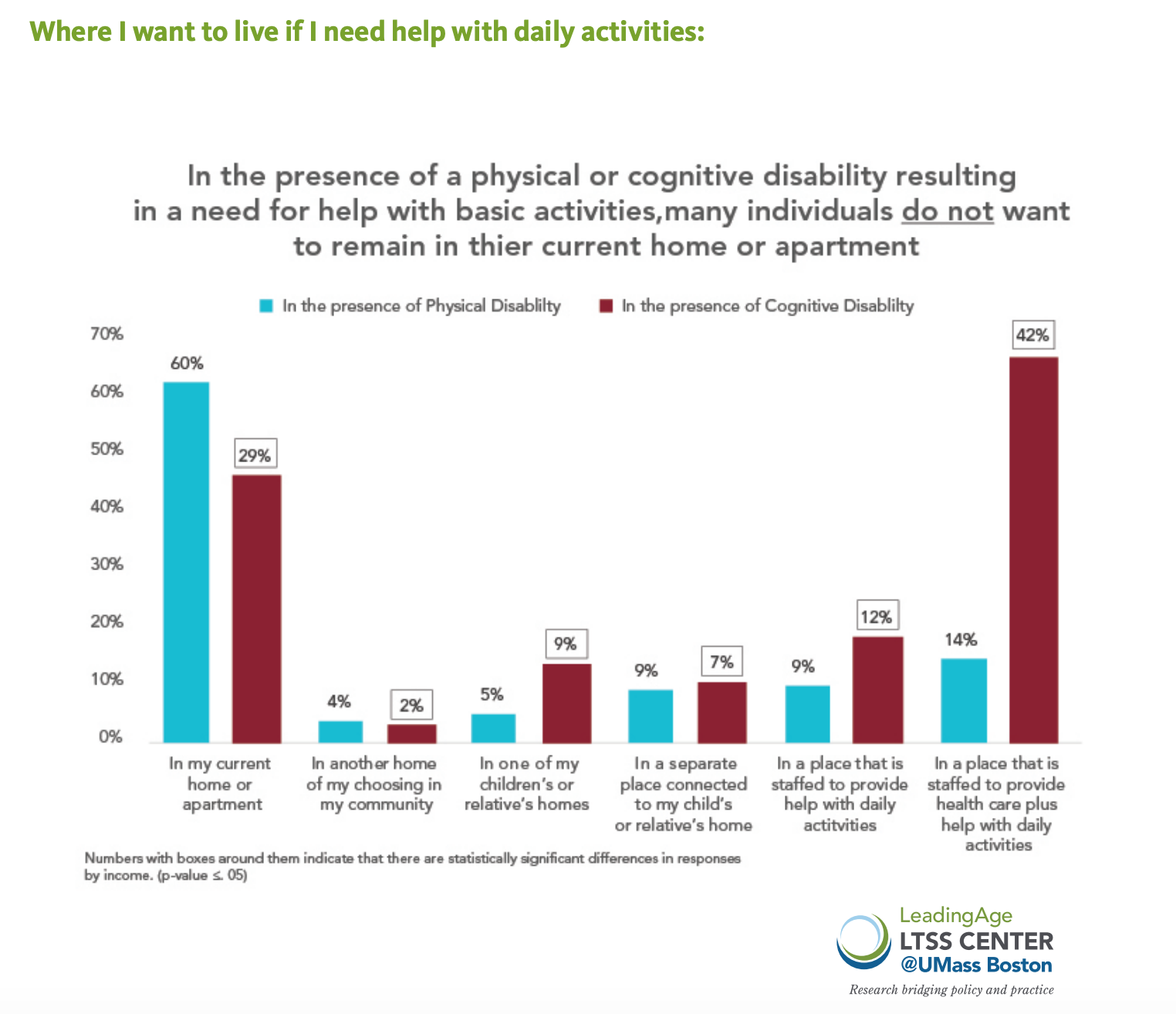
A recent LeadingAge/NORC survey of adults ages 60-72 found 42% would want to live somewhere other than their current home if they had a physical disability or cognitive decline that required them to need help with daily activities. That's what nursing homes and assisted living facilities do.
Our Commitment to Covering the Coronavirus
We are committed to reliable reporting on the risks of the coronavirus and steps you can take to benefit you, your loved ones and others in your community.
Read Next Avenue's Coronavirus Coverage
"There is a real need for these services," said Sanders.
Data crunched by ProPublica for its database of nursing home deficiencies, Nursing Home Inspect, has not found a significant difference between for-profit nursing homes and nonprofit nursing homes as far as which ones close or remain operating.
If a sizable number of nursing homes do close, the most at risk will be the people on Medicaid who make up the majority of the 2.5 million residents in skilled nursing facilities.
"For many Medicaid patients, nursing homes are the only place they have to go," said Mary Haynes, president/CEO of Nazareth Home, which operates two nursing homes in Louisville, Ky. "The federal and state governments have an obligation to serve the frail, the elderly and the disabled. But the COVID-19 crisis has exposed the shortcomings in funding for these populations. Current Medicaid funding levels cannot sustain nursing home operations."
Roughly 60% of nursing home-operator funding comes from Medicaid, which covers 70% to 80% of operating costs. The difference has been made up through Medicare or private-pay health insurance, but that funding has been declining, accelerated by COVID-19.
Fewer older adults have pursued elective surgeries requiring short-term rehabilitation stays in nursing homes. And many patients discharged from hospital ICUs or long-term acute care facilities have been opting for home care, rather than nursing home care, over fears of the COVID-19 infection rates in nursing homes.
"Unfortunately, many skilled nursing facilities were experiencing operational obsolescence even before COVID," said Steier.
AHCA/NCAL has found that more than half of nursing homes are operating at a loss, with nearly one in five beds now going unused. Since COVID-19, 97% of nursing homes have lost revenue due to increased costs for infectious disease equipment and testing, training and labor costs.
The hardest hit are rural areas. And that's after more than 440 rural nursing homes closing or merging over the last decade, according to the Cowles Research Group, which tracks long-term care.
For most nursing home operators, the risks of sustaining their business fall into three categories:
1. Staffing
COVID-19 has required nursing homes to embrace infectious disease protocols and focus equally on minimizing patient risk of transmission and employee health, a structure Haynes believes many don't have.
"The burden on our workforce is tremendous," added Haynes. "We're required to test staff twice a week, but many of our certified nurse assistants are having to drive thirty minutes to come to our offices for a fifteen-minute test and then drive back thirty minutes to get to their place of work."
Some operators said they're spending a year's worth of their PPE budget on just one month of supplies.
While Steier feels many nursing homes are struggling with increased labor costs for "hero pay," he also believes staff working 70-hour work weeks are struggling with being demoralized by the negative media coverage of nursing homes versus the heroism portrayed by acute care hospital workers.
"Nursing homes really took the brunt of negative coverage as COVID unfolded across the country," said Steier. "Certified nursing assistants are the backbone of our workforce, but it's challenging to recruit them when they can find less-demanding jobs in retail or other industries for comparable or better pay."
Charlene Harrington, professor emerita of Social Behavioral Sciences at the University of California, San Francisco, however, told NPR's Ina Jaffe that for-profit nursing home managers have kept staffing low as part of their strategy to make money.
2. Cost of COVID-19 Protective Equipment
In LeadingAge's October "Situation Report," some operators said they're spending a year's worth of their Personal Protective Equipment (PPE) budget on just one month of supplies.
While PPE and COVID-19 tests have been more available lately, they still represent a fragile supply chain. Large hospital systems are stockpiling supplies, especially N95 masks, leaving some smaller nursing home operators without necessary equipment.
More than 25% of nursing homes reported a shortage of things like N95 masks, gloves and gowns recently.
Dr. Kim Perry, senior vice president and chief medical officer for Kindred Healthcare, which operates long-term acute care, rehabilitation services and behavioral medicine in 46 states, said news reports noted that some PPE meant for nursing homes has been stolen off loading docks and instead gone to acute care facilities.
A lot of the supply problems have been driven by state mandates and outdated requirements for prior purchasing habits restricting increased requests.
Prior to the pandemic, nursing homes were slowly adopting technology such as telehealth services but lagged behind assisted living and home care agencies.
3. Technology
"As we weather the second spike of the coronavirus this fall, technology is a key to surviving," said Steier. "Regardless, it will take two years to get to where we were prior to the pandemic."
One organization helping nursing homes get trained on innovative technology is the Thrive Center in Louisville. "The challenge for tech adoption in long-term care is reimbursements from [the federal Centers for Medicare & Medicaid Services]," said Sheri Rose, CEO of the Thrive Center.
Haynes believes the need for nursing homes is, and will remain, enormous.
"We cannot say what families and older Americans will want and need in long-term care, but having choices along the care continuum remains crucial," said Haynes.

Sherri Snelling is a corporate gerontologist, speaker, and consultant in aging and caregiving. She is the author of “Me Time Monday – The Weekly Wellness Plan to Find Balance and Joy for a Busy Life” and host of the "Caregiving Club On Air" podcast. Read More

