Young Blood for Aging Bodies?
In this Ask the Expert column, a Stanford researcher explains the implications
(Editor’s note: This article is part of an editorial partnership between Next Avenue and The American Federation for Aging Research, a national nonprofit organization whose mission is to support and advance healthy aging through biomedical research.)
The prospect of living healthier for longer as we grow older is not just a hope but a reality, thanks to science. Respected researchers are making great strides in how we can extend healthspan — our years of health as we age.
From targeting cellular processes to delaying age-related illnesses, innovations are closer than ever to moving from the labs into our lives. Many bright discoveries are being driven by researchers supported by AFAR, the American Federation for Aging Research.
In addition to regular columns by Scientific Director Steven N. Austad, Next Avenue and the AFAR are excited to share insights from the field of aging research through Ask the Expert interviews.
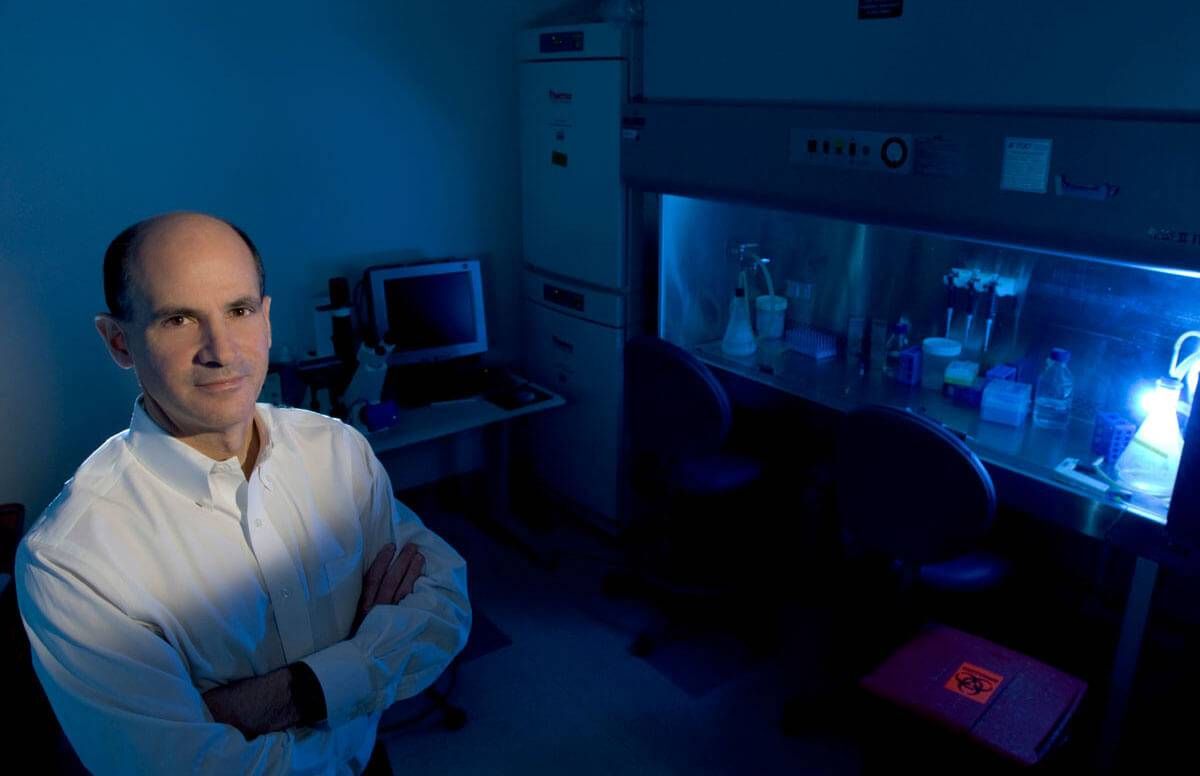
Here, we spotlight Dr. Thomas Rando, whose pioneering research explores how blood from younger animals can apparently rejuvenate the cells and tissues of older animals. Rando is the head of a laboratory at Stanford University, where he is also the director of the Glenn Center for the Biology of Aging, deputy director of the Stanford Center on Longevity and a professor in the Department of Neurology and Neurological Sciences, as well as an AFAR board member and multiple grantee.
We talked with Rando about his research and its implications for human aging:
AFAR: You were the first researcher to discover that blood from young mice could reverse the effects of aging in old mice. What led you to originally pursue that research path?
Dr. Thomas Rando: That path was an extension of the work we were doing looking at tissue aging, which historically had been quite descriptive. Scientists would observe how tissues age and characterize them, but not really get at the underlying mechanisms or causes — at least not in mammals, typically. That has changed dramatically in the past 15 to 20 years, during which aging research has become much more rigorous and experimental, particularly with regard to genetic and pharmacological studies to better understand how to modify the aging process.
We had decided some years before that we were going to use so-called heterochronic techniques. By that, I mean mixing cells or tissues of different ages to test for ways in which the effects of aging might be modified. Typically, that would be done by transplantation. For example, one would take old cells and transplant them into a young animal and ask: When old cells are now in a 'young environment,' do they take on the characteristics of younger cells?
We were interested in trying to push this concept a bit further, and we used another heterochronic technique called 'heterochronic parabiosis'— in which two animals, one that’s young and one that’s old, are surgically connected so they develop a single shared circulatory system, like conjoined twins.
What we observed is that as the cells and tissues of old animals were exposed to circulating blood from the young animals over the course of weeks and months, they started to look younger — as if the cells and tissues in the old animal were actually being rejuvenated. So that really opened up the whole new field.
We and others started to ask: What is so magical about young blood that might benefit old cells and old tissues and maybe old organisms in this way? That started us on the path of trying to understand what is in young blood that has this potential therapeutic benefit and also to try to understand what is actually changing in the old cells, at a molecular level, that makes them seem younger.
The scientific use of blood from young donors to rejuvenate older adults remains controversial. What do people need to know to differentiate the evidence-based, scientific work you and your colleagues in the field are doing from the wild, unsubstantiated claims too often seen in media coverage and advertising?
I would start by saying that there is no evidence that blood donated from young people and given to older people has any health benefit. We’ve seen these benefits in mice, but we don’t know if this is true in humans. Because it’s unproven, anyone who claims that they’re delivering a therapy would be doing so on false premises.
That’s where the controversy comes in. This needs to be tested in bona fide clinical trials. Until we have solid evidence that there really is a proven benefit in humans, I would not recommend to anyone that they receive any blood product based on the prospect that it might have some sort of 'rejuvenating' benefit.
The first small, early-phase clinical trial testing infusions of blood plasma from young donors to people with mild to moderate Alzheimer’s disease last year showed promising results — not only in safety, but in functional ability. What is the significance of those results, and what are the next steps?
This was the clinical trial that was done by the biotechnology company Alkahest in collaboration with Stanford University. I should note that I am on the scientific advisory board of Alkahest. That was a very small trial — 18 patients — conducted over a very short time. It really was designed as a safety trial. In this kind of clinical trial, the first step is to look at safety, and then move on to looking for therapeutic benefit. I would say the main outcome of that trial is that safety was demonstrated.
For the most part, no benefits were noted in most of the outcomes that were measured, including cognitive testing, but there was a suggestion of some improvement in a couple of functional measures. Still, this was really just to assess whether a larger trial to test for efficacy is warranted, and that is being planned now.
You’ve said that identifying reliable biomarkers, or medical signs, in humans is a key to accelerating the field. How close are we to finding those biomarkers?
I don’t think it’s a matter of whether we are close to identifying them. The question is how fast can we advance our ability to use biomarkers that we know of, or ones we have yet to discover, to make them more valuable in clinical trials.
This tends to be a challenge for every field. For any disease, what you want is a rapid, specific, sensitive, reliable, reproducible test — such as a blood test or even something simpler than that — that tells you if your therapy is working. In any field, no matter how good the biomarkers are, there’s always an interest in getting better biomarkers that are faster, cheaper, more accurate, more sensitive, more specific.
So I would say that in the aging field, and this idea of looking at therapies that actually impact the aging process, our biomarkers to date are imprecise and nonspecific. But they’re getting better. It’s really an evolution of ever-improving biomarkers for the things we want to measure, and I have no doubt that these will continue to improve in the years ahead.

