Hot Flashes Aren't Just for Women
Men receiving hormone therapy for prostate cancer often get hot flashes, too
I'm still hot: It just comes in flashes now. It's not a hot flash: It's a power surge.
I don't have hot flashes: I have short, private vacations in the tropics.
As a healthy man, I never paid much attention to jokes like that. Then I got prostate cancer and started having hot flashes myself.
Now I don't find these jokes so funny — and I have a lot more empathy for women who endure these unpleasant spurts of heat. Hot flashes are neither insignificant nor only a "women's problem."
More than two-thirds of North American women who are heading into menopause have hot flashes. They typically experience menopause in their 40s or 50s, but it's not unusual for hot flashes to continue into their 60s or longer. Many women also get night sweats and have trouble sleeping.
Hot flashes are neither insignificant nor only a "women's problem."
Celebrities from Michelle Obama to Gwyneth Paltrow have spoken out about menopause. Wanda Sykes observed in one of her Netflix comedy specials: "Hot flashes are the worst. They're crippling. All of a sudden, you just flop sweat. … There's no way in the world men would put up with hot flashes."
She's right, except for the part about the problem being limited to women.
In fact, men get hot flashes, too, although less commonly than in women. Low testosterone is the main reason. Many men with lower levels continue to feel healthy and happy, but very low levels may cause the hypothalamus — the brain's inner thermostat — to send signals triggering hot flashes.
Hormone Therapies for Prostate Cancer
This is especially likely with some of the hormone therapies commonly used to treat prostate cancer. They reduce testosterone drastically to stop patients from producing new fuel for prostate cancer cells. Most patients end up getting hot flashes, often accompanied by side effects ranging from weight gain to sexual dysfunction.
Many older men can attest to this. More than 265,000 new prostate cancer cases are expected this year alone, according to the American Cancer Society. About six cases in 10 are diagnosed in men who are 65 or older. Upwards of three million men in our country have been diagnosed with prostate cancer at some point and are still alive with the disease. About 34,500 die annually.
Prostate cancer is serious, in other words, but most men diagnosed with it survive, especially if they identify and address the problem early.
That's what my oncologist told me after a blood test and then a biopsy revealed the early stages of prostate cancer last fall. "You're going to die of something else," he reassured me.
He guided me through my treatment options, which were mainly to remove my prostate through surgery or zap it with radiation, together with hormone therapy to restrict my testosterone.
My Experience with Hot Flashes
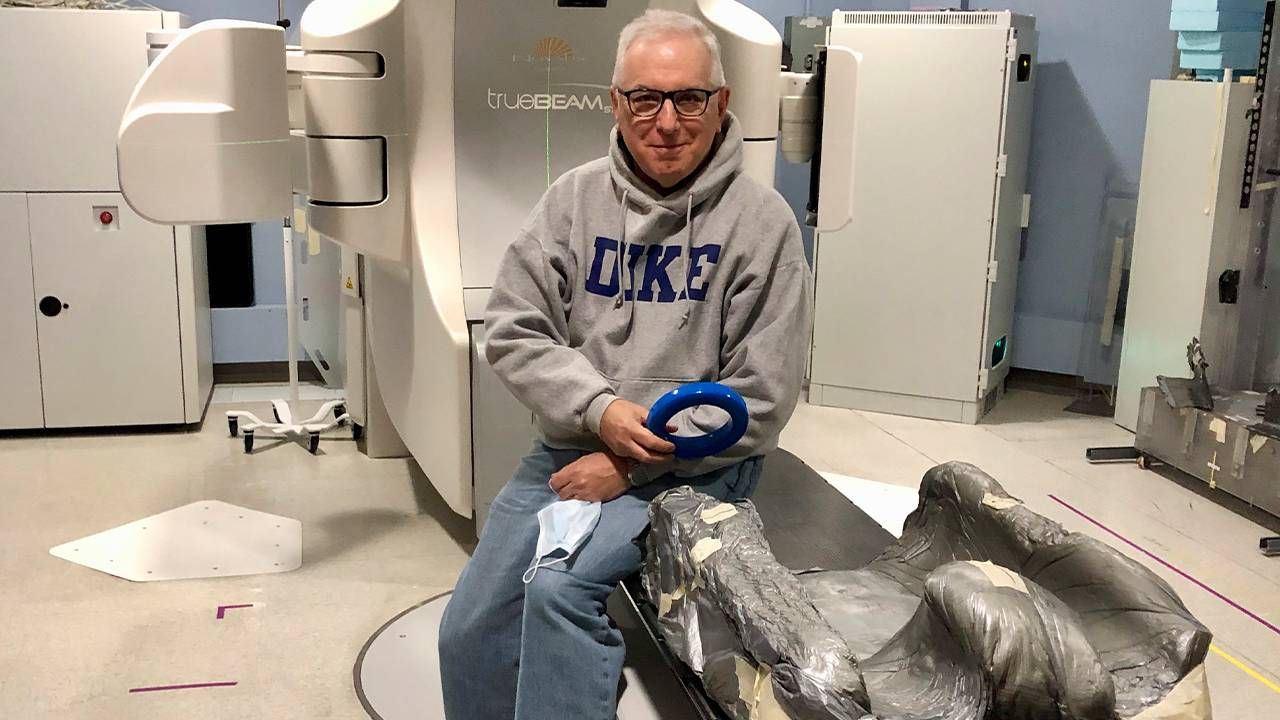
Each option had plusses and minuses. I eventually decided on a combination of radiation and hormone therapies.
I expected the radiation to be worse, but it wasn't, at least for me. I was tired for a few weeks and then bounced back. However, I was among the majority of prostate cancer patients who got hot flashes and fatigue after starting the hormone therapy.
More nights than not, I sweated through my clothing, feeling surges of warmth and twitching from internal temperature changes.
More nights than not, I sweated through my clothing, feeling surges of warmth and twitching from internal temperature changes. I couldn't sleep well and felt drained, even after the radiation ended.
I tried taking herbal supplements that reportedly ease symptoms for some men, but they didn't do much for me. I rejected medications that have shown some success, including antidepressants, because of possible side effects. Instead, I just avoided potential dietary triggers, took daily walks and kept a cool washcloth handy.
I kept reminding myself that my side effects were less severe than I might have faced with deadlier cancers or more intensive treatments. I was lucky to have this particular cancer and to have caught it early, and to have a loving family and a superb medical team at the Duke Cancer Center in Durham, North Carolina. My heart goes out to others who have been less fortunate.
Side effects vary widely among patients, even among those with similar cancers and treatment regimens. In my case, the hot flashes were pretty miserable. I was relieved to recently complete my six-month course of hormone therapy, although it took several more weeks for my body to readjust.
My latest blood test was great. I'm feeling optimistic. And I'm grateful not only to have survived this episode but also to have gained some overdue insight into a health problem I never took seriously enough, even when it affected women in my own family. I hope other men will become more sensitive to it as well.

