What Is a Small Stroke?
After I was diagnosed, I learned a 'small stroke' might indicate a physically small size of damage or a small number of symptoms. Here's what else I learned.
In mid-summer, my partner Susan was concerned. She was sure my behavior had changed in recent weeks and wanted me to get it looked into. I wasn't convinced and consequently was shocked when our doctor told me that my MRI scan showed that I had suffered "a small stroke."
"Not all kinds of stroke symptoms are associated with changes in brain scans [and] not all kinds of things that look like infarcts or damage on brain scans are associated with symptoms."
When he said "stroke," I imagined what I had seen on TV or heard from friends whose parents had suffered strokes: half-paralyzed faces, an inability to talk and perhaps the loss of the use of hands or legs. My doctor was upbeat, but I was stunned. And as I left his office, I had many questions.
Learning More About a Small Stroke
The phrase "small stroke" can mean many things. According to Dr. Thalia Field, a neurologist with the Vancouver Stroke Program and Associate Professor at the University of British Columbia, "stroke" is a clinical term used to describe either symptoms or to refer to a kind of lesion shown on a brain scan. The challenge, she explains, is that "Not all kinds of stroke symptoms are associated with changes in brain scans [and] not all kinds of things that look like infarcts or damage on brain scans are associated with symptoms."
In simple terms, a "small stroke" might indicate a physically small size of damage or a small number of symptoms. "If you have a little small stroke in a quieter area of the brain, like a small area in your right frontal lobe, you may not notice, but if it's in an area where all your motor pathways are passing together, it can be very symptomatic," according to Field.
In my case, the family doctor chose not to use a tool like the National Institutes of Health Stroke Scale (NIHSS), which standardizes a large number of measures of physical and mental damage. Instead, he decided I was basically doing well and just reported my condition as a "small stroke."
"You may be bothered by numbness or dexterity issues. Or your spouse may be noticing that you're not yourself."
However, what your doctor sees as minimally symptomatic might seem much larger to you, the patient. Field says, "Your doctor might say your stroke is small, but you may find that you're not planning things in the same way. You may be bothered by numbness or dexterity issues. Or your spouse may be noticing that you're not yourself."
Will I Have More Strokes?
My next question was whether I would have more strokes or bigger strokes in the future. My family doctor told me that I was "100% certain" to have subsequent strokes. Field was more nuanced.
"Once you've had one stroke, you're more likely to have another, but beyond that, it can be challenging to predict whether a specific individual will have a stroke. Age, lifestyle choices, genetics and other factors play a role, but it's still true that 'there are more people without strokes than with them.'"
The likelihood of a stroke does increase with age, and how strokes present differs between men and women. Women tend to see strokes more often during pregnancy and childbirth and with menopause. Women tend to live longer than men and so are at greater risk of suffering age-related strokes. There are also questions being raised about gender bias influencing treatment choices.
A 2023 study from the University of Texas Health Science Center at Houston found that compared with men, women who had suffered a severe stroke were older and presented with a greater NIHSS stroke score, meaning their symptoms were worse. After adjusting for differences in relevant factors, women with large vessel occlusion acute ischemic stroke were approximately 9% less likely than men to be routed to comprehensive stroke centers.
Regardless of external factors, if you've had one stroke, you're more likely to have another, often within the next 24 hours. Some people are just more prone to having strokes, and it can be hard to say what pattern will emerge. The good news if you've had a minor stroke is that research into secondary stroke prevention is already underway, exploring strategies to prevent strokes from reoccurring over the shorter term.
Medications Help Prevent Future Strokes
I am now on two medications. The first is Clopidogrel, which prevents platelets from sticking together to form harmful clots. It also helps lower "bad" cholesterol and fats (such as LDL and triglycerides) and raise "good" cholesterol (HDL) in the blood.
My stroke was in the right frontal lobe, a part of the brain that deals with memory processing information.
My second pill, Atorvastatin, belongs to a group of drugs known as "statins." They work by reducing the amount of cholesterol made by the liver. Lowering "bad" cholesterol and triglycerides and raising "good" cholesterol decreases the risk of heart disease and helps prevent strokes and heart attacks.
As always, medications such as these bring their risks and side effects. According to the Mayo Clinic website, "It's important to consider your medical reasons, personal values, lifestyle choices, and any concerns when choosing a treatment. Talk to your doctor about your total risk of heart and blood vessel disease and personal preferences before deciding on statin therapy."
Measuring Stroke Damage
How does a stroke sufferer measure their impairment? The common suggestion is to see a neurologist for detailed testing, but according to Field, it's the person who has experienced the stroke who is often the best one to gauge a subtle impairment.
"A neuropsychologist could do really detailed testing, [but] for sensitive measurement you can use your own awareness, or that of someone who is close to you, to notice changes, and this is probably the best measure of subtle impairment."
My stroke was in the right frontal lobe, a part of the brain that deals with memory processing information. The advice from our family doctor was straightforward: plan and avoid last-minute decisions. That advice is reinforced by the Ohio-based Cleveland Clinic, whose website explains that damage to the frontal lobe can include symptoms such as "trouble with reasoning, paying attention, organizing, planning or switching your attention between two tasks."
Still, Field suggests you also get referred to a neurologist to ensure you've been adequately assessed and rule out conditions your GP may have missed.
The Brain Can Repair Itself
There is good news, though: the brain can often repair itself. Even though the damaged area of the brain will remain, neuroplasticity means that the brain can make new neural connections around the damage, learning new ways to handle old tasks.
"Look at your local stroke survivors' groups. It's one thing for your doctor to read about stroke and know what's in the literature and see patients, but it's quite another thing to be living and recovering from it."
Social engagement is also a general predictor of wellness over time. Activities with novelty stimulate your brain, help protect against cognitive dysfunction, help control mood swings, and encourage recovery. Field says, "The mechanisms are not always fully teased out, but certainly social engagement is a positive thing that helps maintain your brain networks and make new connections, and it is a mood booster."
Advice For Someone Recovering From A Stroke
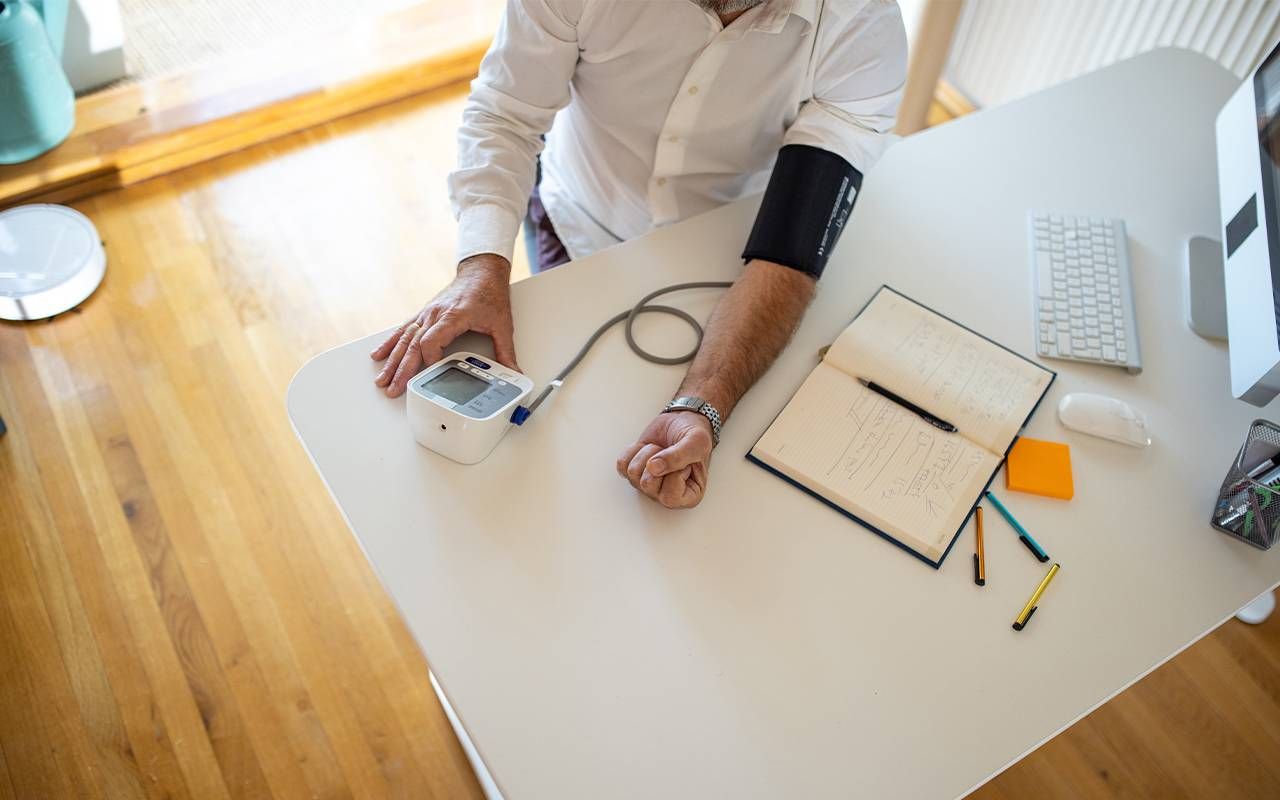
Your small stroke is a good opportunity to reassess your overall wellness and cardiovascular health. Is your blood pressure well controlled? How is your cholesterol, and are there blood sugar or diabetes issues? Do you smoke, and can you increase your level of physical activity? It's also an opportunity to get screened for an irregular heart rhythm like atrial fibrillation, which is associated with a high risk of stroke.
Beyond that, look at risk factors in your lifestyle. Eat a Mediterranean diet, get exercise and be socially active. And look for local stroke support groups. These will allow you to talk to other stroke survivors and learn about your condition from a patient perspective rather than that of a doctor.
Field says, "Look at your local stroke survivors' groups. It's one thing for your doctor to read about stroke and know what's in the literature and see patients, but it's quite another thing to be living and recovering from it. You may be interested to know about someone's recovery trajectory, or maybe they know a really good therapist or perhaps they have some tips for how to reintegrate exercise into your life.
Peer support is a really important thing, and also helps to reduce the sense of isolation that can happen after a stroke. The American Stroke Foundation has an online stroke support group finder on its website.
Going Forward
I've come to accept my stroke diagnosis. I don't like it, and I still worry about subsequent strokes. Still, I also understand that my future depends on how I lead my life, what healthy habits I continue, and how I can build my daily routine around any impairments I have developed.
More importantly, I understand that my small stroke isn't the great, disabling event that I thought it was. It's more of an ongoing nuisance and something that might slow me down, but it doesn't stop me from living a complete life.