Life Lessons from My Grandmother's Death
How the end of my grandmother's life taught my family about the importance of planning
It started with my grandmother not being able to breathe. My grandfather took her to the emergency room. Tests discovered a heart valve wasn't working. After a successful surgery, Grandma recuperated in the ICU.
That night, Grandma's heart stopped. She had a Do Not Resuscitate (DNR) order. They resuscitated her.
Unbeknownst to us, the hospital needed legal DNR documents on file, or they could not follow the order. It didn't matter that my grandmother had put it in her entry paperwork.
She didn't want to be hooked to machines and die in a sterile, harsh hospital.
My whole life, I remember my grandmother talking about the death scene in the movie "Soylent Green." For those who do not know the film, it takes place in a grim, apocalyptic future. When people were ready to die, they went to a facility where they watched images of a beautiful earth while listening to soothing music. They fell asleep and never woke up.
My grandmother said, "That's a good way to die."
She didn't want to be hooked to machines and die in a sterile, harsh hospital.
After they resuscitated her, they intubated my grandmother and hooked her to a ventilator. The doctors wanted to give her a tracheostomy to keep her on the ventilator for an extended period.
My mother knew that wasn't what my grandmother wanted. But the doctors said she would need it only for a couple of weeks. So, my mother said yes.
My grandmother was so angry at my mother. She wouldn't look at my mom for days.
After two weeks, they tried to wean her off the ventilator. Each time they tried, she destabilized.
Eventually, the hospital moved my grandmother to a rehabilitation center. I visited as often as possible. Unable to talk, she would hold my hand, and we would watch TV.
Her Life for Two Months
I was heartbroken seeing Grandma hooked up to machines that beeped and kept her alive. She experienced random pain in her stomach they never diagnosed. Occasionally, she would put her hand on her stomach, and her face would grimace as her mouth said, "Ouch! Ouch!" but no sound came out.
This was her life for two months.
Finally, the doctors discovered half of her heart had stopped working. As the machine pumped air into her lungs, the movement of her lungs pumped her heart for her.
I was there when the doctor came in. "There is nothing else we can do for you," he said to my grandmother. "I understand you'd like to be taken off the machines?"
My grandmother nodded earnestly.
They turned off the machines the next day, and my grandmother passed away. She was 82.
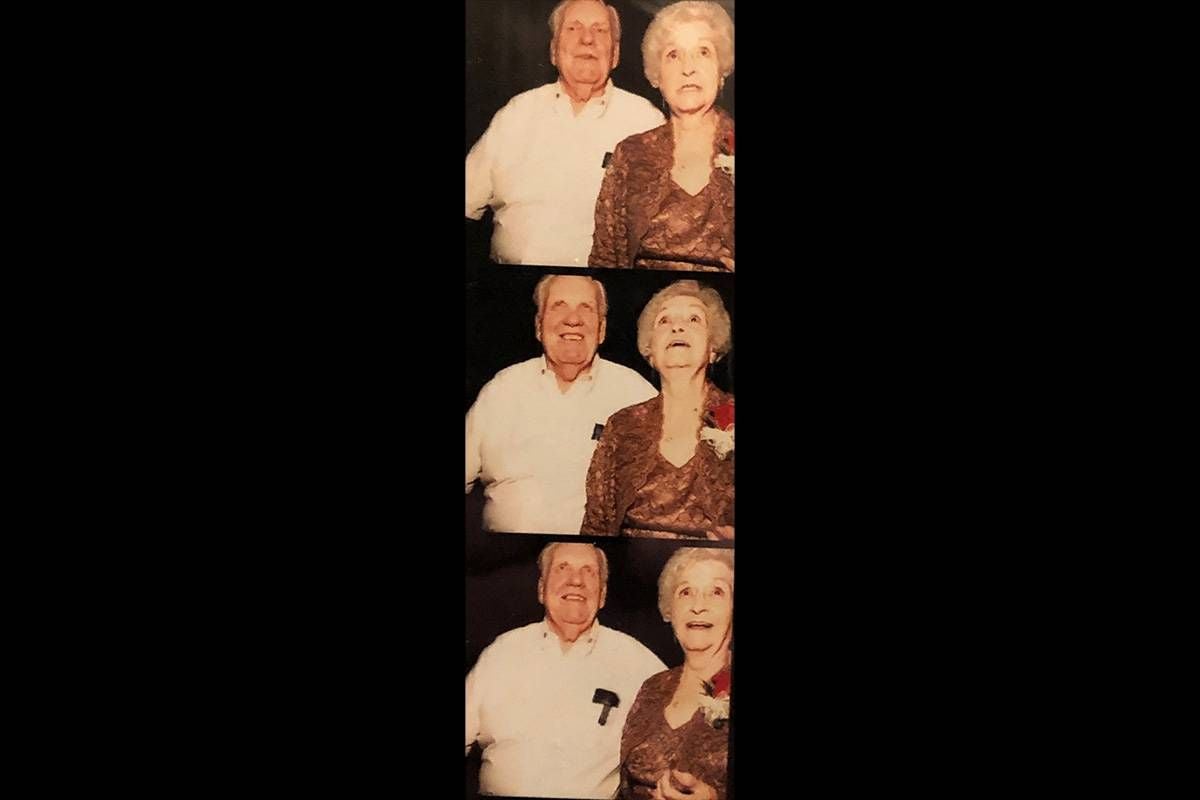
Grandma didn't want a big funeral. We had a memorial gathering in the backyard. We set her picture on a table next to her ashes. It felt like a summer BBQ with a bunch of extended family I rarely see. People milled around drinking beer, eating Costco sandwiches, and talking about sports. There were no speeches, no toasts.
My grandmother's end-of-life journey consisted of miscommunications adding unnecessary pain to an already painful situation.
My mother honored Grandma's wishes, but without ceremony, my mother lacked closure.
My grandmother's end-of-life journey consisted of miscommunications adding unnecessary pain to an already painful situation. Grandma said, "I don't want to be hooked up to machines," and "Don't make a fuss after I am gone." Those two sentences may seem like enough to know someone's wishes. But as my grandmother's story shows, it is not.
Making End-of-Life Plans
No one likes talking about death, especially our own. But I'm here to tell you as we plan for our lives, we must plan for our deaths.
Before we can tell our loved ones our wishes, we must ask ourselves some questions.
What does living mean to me?
If diagnosed as terminal, what are the most important things to keep in my life?
What am I willing to give up in order to keep what is most important to me?
For example, what if Grandma said, "If I can be home watching TV with my husband beside me in his comfy chair, then I won't care about the machines." With that specific information, my mother's decision for my grandmother might have been different.
We need to decide what makes life worth living. Then we must tell our loved ones so they can make decisions for us without doubts.
As for the family members, the challenge is to set emotions aside when making choices for our loved ones. No one wants to make these decisions but finding out their wishes removes the guessing. We may not like their wishes. But when we have solid guidelines on how to make decisions, it is easier to do, even if it breaks our hearts.
Talking to Doctors
The next step is to make sure the doctors follow your wishes.
Decide if you want a DNR and in what circumstances. You'll need to research requirements for a legal DNR in your area. Without that legal paperwork, hospital staff will always do whatever it takes to keep a patient alive. Their job is to keep people alive.
Today's medical advances can keep someone alive longer than was an option before. However, length of life and quality of life are two different things. The definition of quality of life is the patient's opinion. If we ask ourselves the tough questions, we should express that opinion.
If my mom knew to ask the doctor about the odds of Grandma getting off the ventilator, he might have answered 40%. My mother might have made a different decision.
Doctors aren't trained to ask what is essential in a patient's life. They are trained to keep you alive. There is a big difference.
When a doctor suggests administering chemotherapy to extend the life of a cancer patient, we don't think to ask, "Extend how long?" We just hear "extend life." That extension might be two to three months, but only one month without chemo.
We need to ask ourselves what is the better option: two to three months with chemotherapy side effects or one month at home with hospice care keeping you comfortable.
Doctors aren't trained to ask what is essential in a patient's life. They are trained to keep you alive. There is a big difference.
By figuring out 1) what is important to us, 2) what we will tolerate to keep those things, and 3) asking our doctors questions about length and quality of life, we get to choose how our lives end. Isn't that what we all want?
Plans Following Death
After my grandmother's experience, my parents are discussing their end-of-life wishes with my sister and me. Furthermore, they want to hear our wishes for arrangements after they pass.
"I didn't feel any closure from Mom's memorial," my mom said. "So, we want to know what would bring you closure."
"We'll be dead," she added. "We won't care."
Discussing what someone wants after they have passed is essential. They might request a favorite song played or a place to spread their ashes. We want to grant those wishes.
However, "funerals are for the living." When someone requests to keep services simple, they don't want to burden those they left behind. My grandmother knew how much time and money went into funeral services.
Follow the specific memorial requests for your loved ones when you know it's important to them. Add whatever you want to show the love, honor and closure you need.
It was hard watching my grandmother's life end. Now, I recognize her experience was a gift to us. We learned just as we plan for our lives, we must plan for our deaths.


