More Treatment Options for People with Macular Degeneration
New therapies and lifestyle changes can help slow the progression of age-related macular generation
Nearly a decade ago Jane Burdette glanced up from a cross-stitch project and noticed the door frame suddenly looked crooked. "I called my primary doctor who referred me to an ophthalmologist who saw me immediately. She contacted the retina specialist who saw me the same day, diagnosed the problem, and gave me the first injection in the left eye," she said. Her diagnosis: wet age-related macular degeneration (AMD) in her left eye, and dry AMD in her right.
"I would have been alarmed if I had known this was the beginning of a long journey."
Upon diagnosis, Burdette, now in her 70s, says, "I was numb because this happened so fast. I was anxious about getting a shot in my eye. I assumed this would be fixed quickly and I would go on my merry way. I would have been alarmed if I had known this was the beginning of a long journey."
She received injections every 4 weeks (ranibizumab, [Lucentis, Genentech]) until late 2022, when she transitioned to a therapy that extends her treatment to every 14 weeks (faricimab-svoa [Vabysmo, Genentech]). She also takes vitamins made for people diagnosed with moderate to advanced AMD. Now in her tenth year of receiving eye injections, Burdette's wet AMD is now stable and some of her vision has improved.
Sight-Threatening Condition
The diagnosis of AMD affects the center of the retina (the macula), which is responsible for central vision. In a healthy eye, the macula captures detailed information from the center of the visual field, and then a person can read, drive a car, recognize faces, perceive color and contrast, and see fine details, according to the American Macular Degeneration Foundation.
The onset of AMD often begins so slowly that many people may not notice symptoms until the disease progresses or affects both eyes. Initial vision changes can include difficulty seeing in the center of vision needed for reading, cooking or driving; trouble seeing in dim light; and straight lines, like light poles, start to appear blurry, crooked or even missing. Fading and/or changes in the appearance of colors, and difficulty recognizing familiar faces are other signs, according to Prevent Blindness.
Types of AMD
The common forms of AMD are non-neovascular ("dry" or atrophic) and neovascular ("wet" or exudative). Macular degeneration starts as dry AMD progresses slowly over several years. It is classified in 3 stages: early, intermediate and late.
An estimated 1 in 10 Americans aged 50 and older have the early form of AMD
Approximately 85% to 90% of the cases of macular degeneration are the "dry" type, while 10% to 15% are the "wet" type, in which abnormal blood vessels grow in the back of the eye and damage the macula. This less common late form of AMD, also called advanced neovascular AMD, usually results in faster vision loss.
An estimated 1 in 10 Americans aged 50 and older have the early form of AMD and approximately 1 out of every 100 Americans ages 50 and older have the late form, according to a study in JAMA Ophthalmology. Overall, it impacts more than 1 million people in the United States and 5 million people worldwide.
What You Can Do
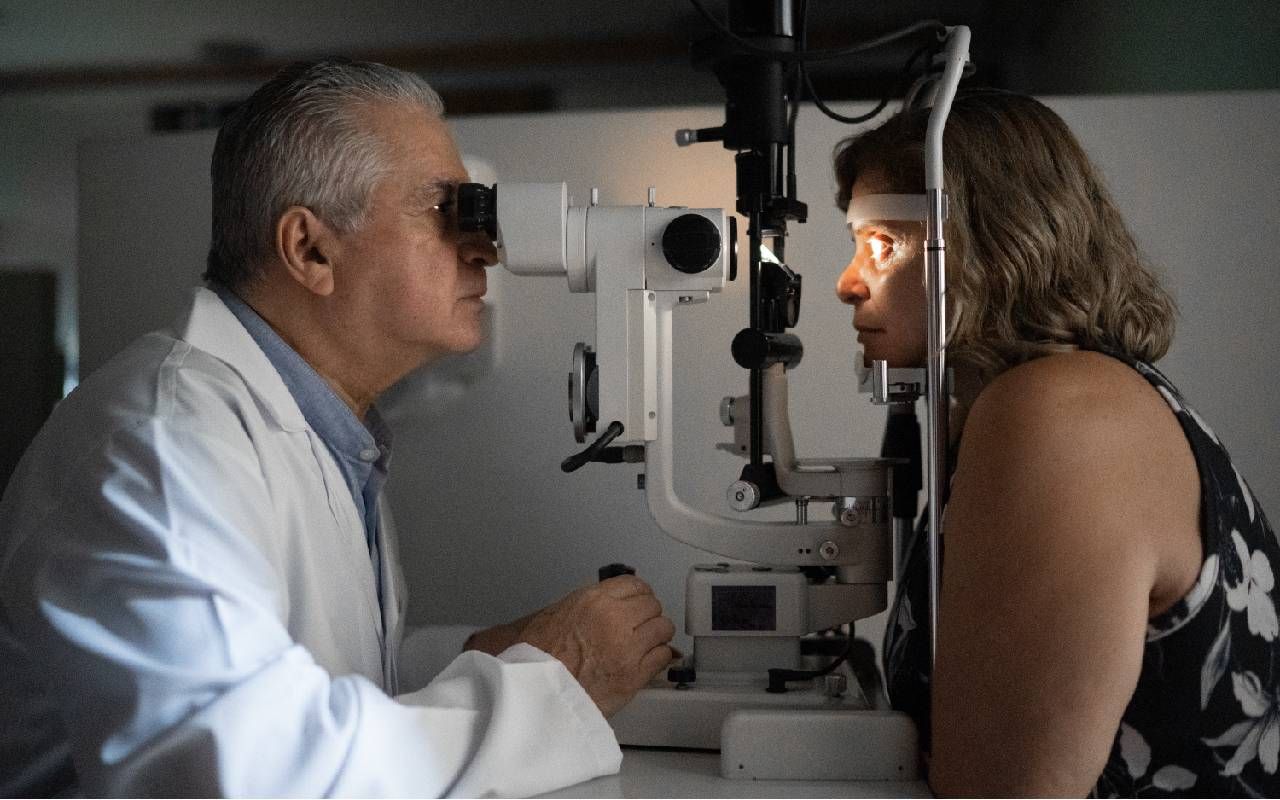
"While we don't specifically have a guideline stating that there is a mandatory requirement for screening from the American Academy of Ophthalmology or the American Society of Retinal Specialists, I recommend patients, particularly those over 65 years of age, get a comprehensive eye exam, which can catch treatable diseases like glaucoma, macular degeneration and diabetic retinopathy at early stages," explains Yasha S. Modi, MD, an ophthalmologist and vitreoretinal surgeon with NYU Langone Health in New York. "Part of that exam is something called a macular optical coherence tomography (OCT) scan, which is an imaging test that's very sensitive at identifying even early stages of macular degeneration."
In addition, lifestyle changes — such as good nutrition and not smoking — can help keep eyes healthy.
"Eating high amounts of leafy green vegetables and low amounts of saturated animal fats is correlated with a lower probability of macular degeneration and less severe stages of macular degeneration. Although we can't prove causality, we tend to recommend diets that are very high in leafy green vegetables and low in saturated animal fats, which is not only beneficial for macular degeneration but can also help with blood sugar and blood pressure control. Overall, this is a very good lifestyle diet," says Modi.
"One of the largest modifiable risk factors is to quit smoking."
"One of the largest modifiable risk factors is to quit smoking. People who smoke are more likely to get macular degeneration or to have their condition progress and worsen. Unfortunately, smoking is highly addictive, so it's beneficial to reach out for help and to use resources available to help quit," he adds.
Treatments for Advance Dry Macular Degeneration
In 2023, the new treatments — pegcetacoplan injection (Syfovre, Apellis Pharmaceuticals, Inc.) and avacincaptad pegol intravitreal solution (Izervay, Astellas Pharma Inc.) — were approved by the FDA to treat geographic atrophy (GA) caused by macular degeneration. GA, the progressive, irreversible, advanced form of dry AMD, is when atrophic lesions form in the outer retina.
"It's important to realize these are not global treatments for all macular degeneration, but rather only for a small population of patients with advanced atrophic macular degeneration," explain Modi.
The treatments, which are given either monthly or every other month in the form of an injection into the eye, slow the progression of macular degeneration, specifically GA.
"We don't know what happens if individuals miss visits, or if they stop these treatments. Additionally, even if you are receiving treatment, it's critical to realize the disease is progressing, albeit at a slower rate. The goal of this treatment is to slow GA before it progresses to the very center of the retina (the fovea)," he says.
"If all goes well, the goal is that over years of receiving these treatments they will still have the ability to see with the center of their retina, because the progression has been reduced."
The pegcetacoplan injection was approved for use for GA with or without subfoveal involvement, with a dosing schedule of every 25 to 60 days. Clinical studies showed that the treatment reduced the rate of GA lesion growth and demonstrated increasing treatment effects over time, with the greatest benefit (up to 36% reduction in lesion growth with monthly treatment) occurring between months 18 to 24 months. Later in 2023, avacincaptad pegol gained approval. Phase 3 clinical studies showed it provided a statistically significant reduction in the rate of GA progression at 12-months.
Modi has used these newer treatments. "Individuals who have extrafoveal (outside of the center of the retina) GA that has progressively gotten worse over time are the perfect patients for treatment. For these patients, the writing is on the wall that eventually the center of the retina will become compromised. Treatment can slow the progression to the fovea that will then ultimately render them with very limited central vision," he explains.
Gauging the real-world impact of treatment can be challenging because there is no measurable output to know the medication is working. "Patients do not see better when they get these injections. If all goes well, the goal is that over years of receiving these treatments they will still have the ability to see with the center of their retina, because the progression has been reduced," he says.
Treatments for Wet AMD
Wet AMD can come on suddenly and insidiously. "That's why we ask all patients to use either an Amsler grid or some form of home monitoring device to be able to detect vision changes at the earliest stages, because the sooner we identify the conversion from dry to wet AMD and start treatment, the better the long-term vision is likely to be," Modi says.
Anti-VEGF agents are used to treat the abnormal blood vessels leaking, growing and bleeding under the retina in wet AMD. Treatments, such as bevacizumab (Avastin, Genentech), ranibizumab, aflibercept (Eylea, Regeneron Pharmaceuticals) and faricimab-svoa, are available to slow the condition's progress and preserve existing vision.
"It's much more important that patients receive consistent anti-VEGF therapy rather than any particular type of anti-VEGF therapy. Oftentimes, patients will miss visits, but the more consistently you receive the injection, the more likely you are to maintain your vision. Your doctor will set out a plan to start the injections typically every 4 weeks and then extend that by some interval based on the response," Modi says.
"Some medications, like faricimab (Vabysmo) or aflibercept 8 mg (Eylea HD), can potentially last longer in the eye relative to other medications and the interval may be extended further relative to first generation anti-VEGF medications. That can lower the number of visits and injections that somebody may ultimately have, and that's huge when it comes to patient satisfaction as well as for the caregivers who don't have to bring them to the office as frequently," he adds.
Less frequently, photodynamic therapy (PDT) is used to treat abnormal blood vessel growth from wet AMD. The drug verteporfin (Visudyne, Bausch + Lomb) is injected into the arm and moves throughout the body to the blood vessels of the eyes. Then focused laser light is directed on the eye's abnormal blood vessels to activate the drug and cause them to close. PDT may improve vision and slow the rate of vision loss. Re-treatments are sometimes needed to treat the blood vessels that reopen over time.
Quality of Life
Treatment has improved Burdette's quality of life and lets her remain active with her community's Historic Preservation Committee. "If I lost the ability to do this work, it would be a great loss for me," she says.
Burdette also encourages others to keep up with their regular eye appointments. "I tell my family and friends to find a good ophthalmologist, one who keeps up with the latest research on AMD, and ask about this disease and treatment options now, before you are diagnosed with it," she says.
Modi points out that probably everyone is touched in some way by a family member or friend who has macular degeneration. "As we are fortunate enough to live longer and longer, this is going to become something that is more prevalent in our society. It's incumbent on everybody over 50 years of age to educate themselves on the warning signs of macular degeneration."


